Clinical phenotypes
Basement membranes are essential for complex multicellular life. Predictably therefore, in humans, there are many pathologies caused by abnormalities in basement membrane proteins. We attempt to highlight a few well described pathologies; not to be exhaustive, but to provide an insight into the complex clinical manifestations of basement membrane disorders and how further research into the basic science underpinning this field may revolutionise treatment.
Clinical manifestations vary widely but can be, in part, attributed to the heterogeneity of basement membranes in different tissues. The following, where possible, will try to classify these diseases by their major organ specific manifestations in order to help facilitate understanding. However, most of these diseases present as multisystem disorders and clinical manifestations vary widely per individual patient, attention is drawn to two classic multisystem disorders in the last section of this summary.
On this page:
The skin
The brain
The eye
Musculoskeletal
The kidney
Multi-system disease
The skin
Epidermolysis bullosa
Epidermolysis bullosa (EB) is a group of rare, complex and genetically varied conditions which presents as blisters, erosions and scarring to the skin. It includes over 30 inherited conditions which are all typified by mechanical fragility. Over 20 different structural skin proteins are affected and amongst these are the basement membrane components laminin(332) and collagen(VII).
Junctional Epidermolysis Bullosa (JEB), a subtype of EB, is characterised by mutations in the genes encoding the three subunits of laminin-332 (LAMA3, LAMB3 and LAMC2), a key basement membrane component. It is characterised by diminished epidermal-dermal adhesion that leads to fragile skin, mechanically inducible blisters on the skin and mucosal membranes, and a series of extracutaneous manifestations and complications.
Presentation is varied but includes the following key features:
- Recurrent blisters or erosions
- Poorly healing wounds
- Early onset of cutaneous signs (in some subtypes)
- Scarring
- Dystrophic nails
- Enamel hypoplasia
- Upper airway disease
Diagnosis often depends upon recurrence of features, early onset and a strong family history. Immunofluorescence antigenic mapping is performed on cryopreserved skin to separate the condition into the subtypes – failing this electron microscopy has a role.
Management involves the prevention of new lesions, enhancing wound healing and managing complications. This is most often with dressings, topical antimicrobials, lifestyle interventions and managing the psychological manifestations of severe cutaneous disease. There is no directed targeted treatment available.
Resources
- Hereditary epidermolysis bullosa. Laimer, M et al. J Dtsch Dermatol Ges. 2015 Nov. PMID: 26513070
- Epidermolysis bullosa – Symptoms, diagnosis and treatment | BMJ Best Practice. https://bestpractice.bmj.com/topics/en-gb/744.
- Laminin 332 in junctional epidermolysis bullosa. Kiritsi, D et al. Cell Adh and Migr. 2013 Jan 1. PMID: 23076207
The brain
Poretti-Bolthauser syndrome
Poretti-Bolthauser syndrome, first described in 2014, is an autosomal recessive cerebellar dysplasia caused by homozygous and compound heterozygous variants in LAMA1 gene (which encodes for the Laminin α1 chain – a key component of basement membranes). Clinically these patients present with non-progressive cerebellar ataxia and intellectual disability. On neuroimaging patients are characterised by cerebellar dysplasia with cysts and an abnormal fourth ventricle. Hypoplasia of the cerebella vermis and mild brainstem abnormalities have also been noted. Ocular motor abnormalities and myopia are also common.
Resources
- Ataxia, intellectual disability, and ocular apraxia with cerebellar cysts: A new disease?. Poretti, A et al. Cerebellum. 2014 Feb. PMID: 24013853
- Mutations in LAMA1 cause cerebellar dysplasia and cysts with and without retinal dystrophy. Aldinger, KA et al. Am J Hum Genet. 2014 Aug 7. PMID: 25105227
- Clinical, neuroradiological and molecular characterization of cerebellar dysplasia with cysts. Micalizzi, A et al. (Poretti-Boltshauser syndrome). Eur J Hum Genet. 2016 Aug. PMID: 26932191
The eye
Knobloch syndrome
Knobloch syndrome is a recessive disorder presenting with vitreoretinal degeneration, retinal detachment, high myopia, occipital encephalocele, and lens subluxation. The disease is caused by variants in the gene COL18A1. This leads to a lack of collagen XVIII in basement membranes. An inference to be drawn from this disease is that collagen XVIII is likely to play a key role in angiogenesis. It is also likely collagen XVIII plays a role in the assembly, maintenance, structural integrity or cellular binding properties of basement membranes.
Resources
- Molecular and clinical findings in patients with knobloch syndrome. Hull, S et al. JAMA Ophthalmol. 2016 Jul 1. PMID: 27259167
- Lack of collagen XVIII/endostatin results in eye abnormalities. Fukai, N et al. EMBO J. 2002 Apr 2. PMID: 11927538
- Persistence of fetal vasculature in a patient with Knobloch syndrome: Potential role for endostatin in fetal vascular remodeling of the eye. Duh, EJ. Ophthalmology. 2004 Oct. PMID: 15465551
Musculoskeletal
Mersosin-deficient congenital muscular dystrophy
Mersosin-deficient congenital muscular dystrophy (LAMA2-related muscular dystrophy) is the most frequent form of early onset, fatal congenital muscular dystrophy. This disease is caused by variants in the LAMA2 gene. This encodes for laminin-α2, a basement membrane component. Within skeletal muscle, the basement membrane is crucial for muscle fibre stability and signal transduction.
This disease presents with poor muscle tone and weakness at birth. In the first few weeks after birth some infants have feeding difficulties and breathing difficulties due to poor muscle tone. Motor development is delayed and limited. Few infants will be able to walk unassisted. Neurological symptoms include seizures. Treatment generally focuses on managing the individual signs and symptoms of the condition.
The prognosis of this condition is poor, as many affected children do not reach adolescence.
Resources
- Congenital muscular dystrophy type 1A | Genetic and Rare Diseases Information Center (GARD) – an NCATS Program.
Schwartz Jampel syndrome (SJS) type-1
Schwartz Jampel syndrome (SJS) type-1 is a rare autosomal recessive musculoskeletal disease caused by variants in the HSPG2 gene (encoding perlecan). Perlecan is an integral proteoglycan of basement membranes ubiquitously expressed throughout the body. The syndrome is characterised by skeletal muscle abnormalities, growth defects, chondrodystrophy and chondrodysplasia, and ocular and facial abnormalities that usually become apparent during childhood. Neuromyotomia is associated with congenital peripheral nerve hyperexcitability. Treatment of SJS aims to reduce muscle stiffness and cramping. Most individuals with SJS have a near normal life expectancy.
Resources
- Perlecan, the major proteoglycan of basement membranes, is altered in patients with Schwartz-Jampel syndrome (chondrodystrophic myotonia). Nicole, S et al. Nat Genet. 2000 Dec. PMID: 11101850
- Structural and functional mutations of the perlecan gene cause Schwartz-Jampel syndrome, with myotonic myopathy and chondrodysplasia. Arikawa-Hirasawa, E et al. Am J Hum Genet. PMID: 11941538
- Schwartz Jampel syndrome | Genetic and Rare Diseases Information Center (GARD) – an NCATS Program.
The kidney
Alport Syndome
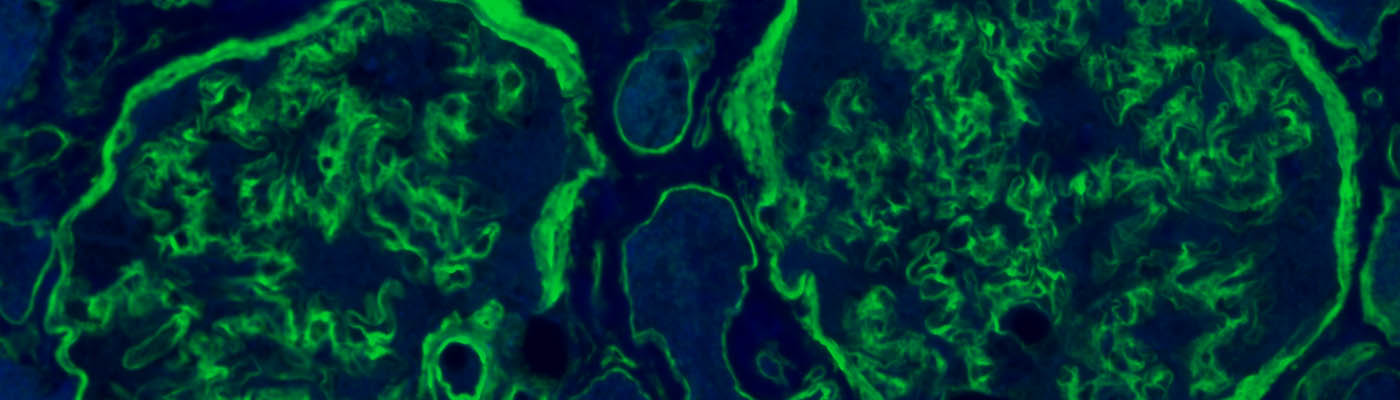
Alport syndrome is caused by variants in genes encoding type IV collagen: specifically, COL4A3-5, that forms the collagen IV-α3,α4,α5 network, which constitutes an important part of the glomerular basement membrane. This is a basement membrane in the kidneys that forms part of the glomerular filtration barrier. Abnormalities in these chains leads to ultrastructural damage to the basement membrane. Collagen IV α3,α4,α5 networks are also found in Descemet’s membrane in the cornea, Bruch’s membrane separating the choroid membrane from the retina, the anterior lens capsule, the lung and the cochlea. The organ specific distribution of these proteins helps to explain the clinical manifestations of the syndrome. Classic features include haematuria, proteinuria, hearing loss, hypertension and kidney failure.
Diagnosis: Positive family history of haematuria with or without progression to chronic kidney disease; progressive sensorineural hearing loss; characteristic ocular changes (anterior lenticonus/maculopathy); typical ultrastructural changes in the glomerular basement membrane; electron microscopy findings include irregular thickening and thinning of the basement membrane; splitting of the basement membrane and lamellation. Genetic diagnosis can confirm mode of inheritance, predict phenotype and help in family planning.
Management is to delay the progression of kidney disease, to treat extra renal manifestation and to offer genetic counselling to family members. ACE inhibitors have been found to reduce proteinuria and delay transplant by more than 10 years. Unfortunately, as of yet, there is no targeted management and definitive management remains a kidney transplant.
Prognosis: Over 90% will develop kidney failure before 30 years of age if they have a loss-of-function mutation in COL4A5.
Resources
- A review of clinical characteristics and genetic backgrounds in Alport syndrome. Nozu, K et al. Clin Exp Nephrol. 2019 Feb. PMID: 30128941
- Basement membrane defects in genetic kidney diseases. Chew, C and Lennon, R. Front Pediatr. 2018 Jan 29. PMID: 29435440
- Alport syndrome – Symptoms, diagnosis and treatment | BMJ Best Practice
Anti-GBM disease
Goodpasture disease presents as haematuria, proteinuria, rapidly progressive glomerulonephritis and lung haemorrhage. The kidney phenotype alone is known as anti-GBM disease, the pathology of which is an autoimmune disease where auto-antibodies are generated against the type IV collagen a3 chain present in the glomerular basement membrane. When these autoantibodies affect the collagen a3 in the alveoli it can result in pulmonary haemorrhage – a presentation eponymously known as Goodpasture syndrome.
Management involves urgent aggressive treatment with high dose corticosteroids, plasmapheresis and oral cyclophosphamide. Pulmonary haemorrhage can be rapidly fatal.
Resources
- Anti-glomerular basement membrane disease. McAdoo, SP and Pusey, CD. Clin J Am Soc Nephrol. 2017 Jul 7. PMID: 28515156
- Goodpasture’s autoimmune disease – A collagen IV disorder. Pedchenko, V et al. Matrix Biol. 2018 Oct. PMID: 29763670
- Goodpasture’s disease – Symptoms, diagnosis and treatment | BMJ Best Practice
- Diffuse alveolar haemorrhage – Goodpasture syndrome | Radiology Case | Radiopaedia.org
Pierson Syndrome
Also known as microcoria-congenital nephrotic syndrome, is caused by homozygous or compound heterozygous mutations in LAMB2. This gene encodes for the laminin β2 chain. This is part of the major laminin isoform laminin-521. Pierson syndrome presents with nephrotic syndrome present at birth (with a histological finding of mesangial sclerosis) and distinct ocular abnormalities and neurological deficits. Similar to Alport syndrome management aims to reduce blood pressure and albuminuria but this is not a long-term cure. Prognosis is generally poor with kidney failure in the first year of life common.
Resources
- Alport syndrome and Pierson syndrome: Diseases of the glomerular basement membrane. Funk, S et al. Matrix Biol. 2018 Oct. PMID: 29673759
Multi-system disease
Many of the conditions already discussed are great examples of multi-system disorders. Type IV collagen-α1,α1,α2 disorders and Fraser Syndrome, are multi-system disorders of which the complexity of their presentations warrants discussion in a separate manner to those discussed by major system affected (as the diseases preceding have been classified).
Type IV collagen-α1α2α1 disorders
These disorders are typically characterised by cerebral vascular defects, eye development defects, myopathy and renal pathology. Gould syndrome is merely one of the presentations of COL4A1/2 related disorders. COL4A1/2 encode type IV collagen α1/α2 chains. These are key components of nearly all basement membranes; the complexity of their clinical presentations attests to this. Although this summary has focused upon Gould syndrome, other related COL4A1/2 disorders are listed below:
- HANAC syndrome: hereditary angiopathy, nephropathy and cramps
- POREN1: autosomal dominant type 1 porencephaly
- Retinal artery toruosity. Brain small vessel disease with or without ocular abnormalities
- Brain small vessel disease with or without ocular abnormalities
- Increased susceptibility to intracerebral haemorrhage
- Schizencephaly
This range of clinical manifestations of genetic mutations in 2 key genes highlights an interesting point. Due to a range of effects different types of genetic variants may have (nonsense vs. splice vs. point etc.), variable penetrance of genetic disease and in some cases the compound deleterious or protective effects other genetic variants may have upon a phenotype; a traditional method of diagnosis based upon merely symptoms may not be beneficial. In these cases, perhaps a molecular diagnosis could be more helpful for prognosis.
Resources
- Gould Syndrome.
- COL4A1/A2-Related Disorders – NORD (National Organization for Rare Disorders).
- COL4A1 mutations and hereditary angiopathy, nephropathy, aneurysms, and muscle cramps. Plaisier, E et al. N Engl J Med. 2007 Dec 27. PMID: 18160688
- COL4A1 mutations as a monogenic cause of cerebral small vessel disease: A systematic review. Lanfranconi, S and Markus, HS. Stroke. 2010 Aug. PMID: 20558831
- COL4A2 mutations impair COL4A1 and COL4A2 secretion and cause hemorrhagic stroke. Jeanne, M et al. Am J Hum Genet. 2012 Jan 13. PMID: 22209247
